Northern California Social Care Summit: Highlights from the Golden State
We were thrilled to bring together so many dedicated leaders from healthcare systems, community-based organizations (CBOs), and public health departments for our Northern California Social Care Summit. The day was filled with energy, candid conversations, and a powerful, shared commitment to building a more connected social care ecosystem for all Californians.
A special thank you to all our attendees and incredible speakers for sharing their insights. The path to navigating complex policies like CalAIM and addressing statewide needs is built through the collaboration and innovation we saw on display.
Read on for key takeaways:
Sutter Health shared its successful pilot that integrated social needs screening in mental health care by leveraging EHR data and staff training.
A CalAIM panel stressed breaking down silos, forming true CBO partnerships, and using Community Health Workers (CHWs) to build trust.
Another panel highlighted essential CBOs, like Rosarium Health and Mom’s Meals, providing critical “boots on the ground” community services.
Highlights from the 2025 California Social Care Summit
This year’s Summit featured 32 participants from 22 organizations across Northern California, representing county government, health care, nonprofits, and more.

A sincere thank you to all our speakers and attendees for a day filled with candid conversation and a shared commitment to strengthening the social safety net for every Californian.
Below are some of the key themes and takeaways from a day of learning and sharing.
Our vision for a connected California
The California Social Care Summit kicked off with a look at Findhelp’s vision for an end-to-end social care ecosystem. We highlighted our full suite of tools—Findhelp, Kiip, SchoolCare, and our benefits eligibility platform, Uno—and how they work together to create a seamless social safety net.
We explored the expansion of our platform into a unified digital infrastructure, from identifying social needs, coordinating services, and managing benefits enrollment to service fulfillment and specialized networks for post-acute care and behavioral health. This allows partners to not only refer but also authorize, manage claims, and process reimbursements for services, all in one place—a critical function for 1115 Waiver work like CalAIM.
The impact in California is already immense:
- 8 million users across the state
- 20 million searches logged
- A powerful spike in searches for housing and food during the Los Angeles-area fires, demonstrating the network’s vital role as a real-time crisis response tool.
We are actively supporting California’s landmark policies, including CalAIM, Governor Newsom’s Children and Youth Behavioral Health Initiative (CYBHI), and SB 660: California Health and Human Services Data Exchange Framework, to help build the integrated infrastructure the state needs.
From the ground up: Sutter Health’s patient-centered pilot
Juan Carlos Piña, Program Manager at Sutter Health, provided a transparent, on-the-ground look at how a major health system begins their social care journey. Grounding his presentation in the fact that 80% of health is tied to social needs, Juan Carlos detailed Sutter’s multi-year strategy to drive quality by building the right infrastructure.

Sutter’s pilot at the Center for Psychiatry focused on a core goal: leveraging Findhelp to connect adult acute care patients with mental health diagnoses to the right community programs. This group is 2x less likely to be screened, but 2.5x more likely to screen positive, highlighting a major service gap.
Key successes and takeaways:
- A Clear Strategy: Sutter’s approach followed a linear path:
- Build the infrastructure via EHR workflows
- Collect data via screening forms
- Populate dashboards with analytical insights
- Inform interventions
- Data-Driven Focus: Early data from the pilot was compelling. Of 1,355 eligible patients, more than 1,000 completed screeners, and of those 227 (20%) screened positive for at least one social need.
- Building CBO Partnerships: Juan Carlos emphasized that community engagement “takes time and should be done well.” His team identified 26 key CBOs and prioritized them in phases, starting conversations with a “less is more” email approach to build trust and assess capacity.
To ensure staff were prepared, Sutter Health’s leadership mandated a 25-minute training module. The result was a 97% completion rate, empowering staff across the hospital to understand and effectively use the Findhelp platform.
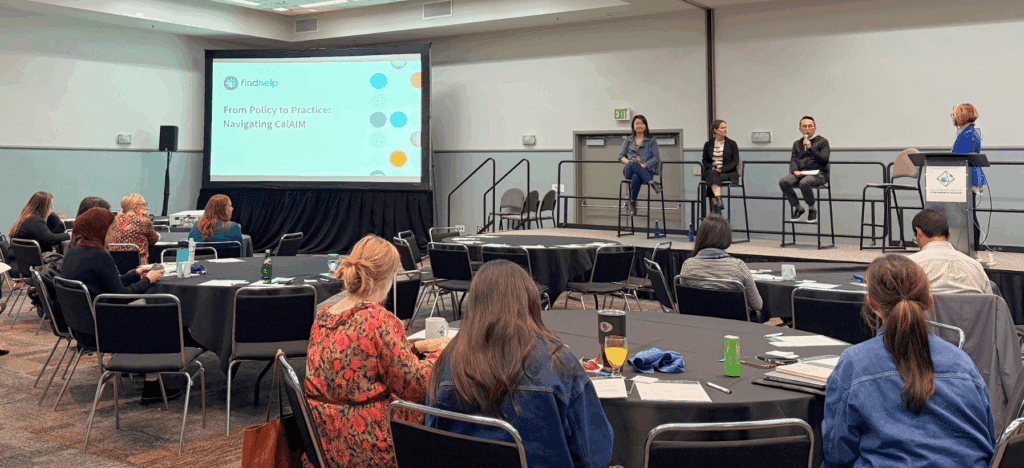
From policy to practice: Navigating CalAIM and CBO partnerships
Our next panel dove straight into one of California’s most significant and complex initiatives: CalAIM. We heard from leaders at the San Francisco Department of Public Health and San Francisco Health Plan (SFHP).
The discussion focused on the central challenge: breaking down historic silos to build a truly person-centered system.
Key themes:
- Building True Partnerships: Tina Yu of SFHP stressed that they seek partners with a trusted community reputation and vital cultural and language competencies. The panel discussed moving beyond a “contracted provider” mindset to one of true partnership, with managed care organizations (MCOs) working together to streamline processes for CBOs. SFHP used a dedicated team to establish CBOs as genuine “partners” and demonstrate a mutual, long-term commitment.
- Barriers to Working Together: The primary barrier to trust and collaboration is the historical disconnect and lack of a “common language” between social organizations and health plans, which requires proactive communication to establish a shared understanding and align on common goals.
- The Power of CHWs: The panel affirmed the essential role of Community Health Workers (CHWs) with lived experience in building trust, especially with members who “have negative experience with their health plans.”
Community organization spotlight: Local partners leading social care innovation
This panel highlighted several CBOs who participate in CalAIM as service providers, partnering with MCOs and the state to meet the needs of Medicaid members. From providing cognitive support for the elderly, complex home modifications, culturally-competent cancer support for the LGBTQIA+ community, and medically-tailored meals for hard-to-reach (e.g., rural) individuals, these CBOs are making a difference in Northern California.
Key themes:
- Simplifying System Navigation: Health and social benefits are “incredibly hard to navigate”; these organizations act as essential partners to streamline complex processes, overcome bureaucratic hurdles (like documentation or landlord consent), and manage the “whole person” rather than a single problem.
- Emphasis on Personalized, High-Touch Support: The presenters championed a “trusted and personal” community-embedded approach—such as visiting every client or using humor to build trust—to counter impersonal systems and meet the unique needs and family dynamics of each individual.
- Findhelp as Critical Infrastructure: The panelists consistently identified Findhelp as the essential technology partner that solves a primary challenge for CBOs: being found. It acts as the “answer” for connecting with social workers, health plans, and more to manage shared referrals and clients.

Powering a smarter, more connected safety net
The California Social Care Summit concluded with a look at the technology that powers this ecosystem. We highlighted Kiip, our free case management platform for CBOs. We’ve full integrated Kiip into Findhelp, with features like a document locker and chat rooms so navigators can communicate with clients.
We also explored the tools that enable the complex work discussed all day:
- Payment functionality to manage claims and reimbursements for waiver programs like CalAIM.
- Payer match capabilities and membership status widgets to help navigators find in-network services.
- Findhelp Coalitions, which create a shared longitudinal social care record to reduce duplicative efforts and provide a true whole-person view.
Beyond the Summit: Our work in California
Our network spans the entire Golden State and individuals across the region use the Findhelp platform to find and connect to needed services and support.
- 23,000 listed programs serving California
- 9.3 million users
- 23.1 million searches for resources
- 117,000 social needs assessments completed
As of October 2025, Findhelp partners with more than 89 customers throughout the state to connect their patients, members, students, constituents, and clients to local resources. Our data and analytic tools can identify gaps in services and provide actionable insights to inform strategy and public policy.

Building a better future for Californians, together
The Northern California Social Care Summit was a powerful reminder that while the policies are complex, the mission is simple: to connect people to the help they need.
The conversation doesn’t end here. To learn more about how Findhelp can support your CalAIM strategy and community, connect with our team.