Meet the Social Care Needs of Medicaid Beneficiaries
There’s been a lot of commentary and discussion recently about Medicaid enrollment and redetermination. What does it mean for your organization and the people you serve? Read on to learn more about the challenges facing healthcare organizations, and the technology solutions that can help you meet the social care needs of Medicaid beneficiaries.
Medicaid: Supporting Vulnerable Populations
Medicaid is a federal program managed by the Centers for Medicare and Medicaid Services (CMS) and implemented by individual states that provides health coverage to low-income people. In the wake of the COVID-19 pandemic and the end of the federal public health emergency, state Medicaid agencies are undergoing a process of redetermination, updating the eligibility status of millions of Americans.

Many people will end up losing their coverage, exacerbating already tenuous situations and increasing the need for community and social services to fill in the gap.

Addressing Social Needs via 1115 Waiver Programs
Section 1115 of the Social Security Act gives states flexibility to design and improve their Medicaid programs by providing waivers authorizing experimental, pilot, or demonstration projects. 1115 waivers are initially approved for five years and can be extended for three to five more years. Many states focus their projects on addressing Medicaid enrollees’ unmet health related social needs and the downstream health impacts.
At Findhelp, we have a history of successful 1115 waiver program support:
California
On January 1, 2022, the California Department of Health Care Services launched the California Advancing and Innovating Medi-Cal (CalAIM) program, an 1115 waiver program to make Medi-Cal more equitable, coordinated, and person-centered. The program covers one-third of Californians and perinatal care for half of annual births and will impact the lives of over 14 million Californians.
New York
The Empire State is awaiting approval on a several billion dollar New York 1115 waiver proposal to invest in creating major social care network structures. We look forward to collaborating with our existing customers and community partners to advance the work of the New York State Department of Health to connect people in need to the programs and services that can help them.
Update: Findhelp is partnering with several Social Care Networks (SCNs) as part of the approved 1115 waiver.

Massachusetts
In response to increasing needs surrounding food, housing, and behavioral health, Massachusetts’ department of health, MassHealth, launched their 1115 demonstration waiver program, Flexible Services, in 2019. Today, we partner with several ACOs to support navigation assistance; in the first year of the Flexible Services initiative, 99% of patients reported that their participation improved their overall health.
Meeting Immediate Needs: Findhelp’s Marketplace
Even if your state isn’t currently implementing an 1115 waiver, you have options to address your population’s health-related social needs. Our Marketplace program allows you to order goods and services from a vetted vendor, deliver them to an individual in need, track outcomes, and manage invoicing and payment – all from your Findhelp platform.
Healthcare organizations and health plans are looking beyond medical needs to improve health outcomes by either paying directly for social care services or reimbursing healthcare groups for arranging them. The government is supportive of these measures, providing grants and allowing Medicare to begin reimbursing plans for “non-medical” services as part of the 2020 CHRONIC Care Act.
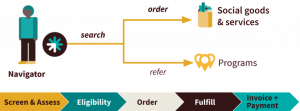
With Marketplace, we’re shifting the paradigm beyond search and referral to order and delivery. We support eligibility and/or authorization of services, order and fulfillment, invoicing, and payment. You can ensure that people who need transportation can order an Uber Health ride to their appointment, or someone who is identified as food insecure gets a food box delivered right to their door.

Navigating the Medicaid Landscape
To learn more about how we support healthcare organizations, health plans, government agencies, and community organizations grappling with the changing Medicaid landscape, connect with us.