Medicaid Waivers by State: Findhelp and California
Section 1115 of the Social Security Act gives states flexibility to design and improve their Medicaid programs by providing waivers authorizing experimental, pilot, or demonstration projects. 1115 waiver programs are initially approved for five years and can be extended for to three to five more years.
Many states focus their projects on addressing Medicaid enrollees’ unmet health related social needs and the downstream health impacts. Findhelp has extensive experience supporting 1115 programs in states like Massachusetts and California, where managed care organizations (MCOs) and accountable care organizations (ACOs) use our platform to place orders for their Medicaid members for reimbursable goods and services. Our technology supports:
- Capturing eligibility and authorization needs
- Reporting on services rendered, codes, and data needed for invoicing and claims
- Invoicing paying entities and facilitating payment to community organizations and vendors
Medicaid 1115 Waivers in California: CalAIM
On January 1, 2022, the California Department of Health Care Services launched the California Advancing and Innovating Medi-Cal (CalAIM) program, an 1115 waiver program to make Medi-Cal more equitable, coordinated, and person-centered. The program covers one-third of Californians and perinatal care for half of annual births and will impact the lives of over 14 million Californians.

CalAIM expands community-based approaches to addressing complex care for high-needs populations, such as individuals experiencing homelessness, serious mental illness, or substance use disorders, or children involved in the child welfare system. Designated navigators coordinate members’ physical and behavioral care, as well as access to critical social services.
Through 14 services such as Asthma Remediation and Housing Navigation Support, CalAIM encourages Medi-Cal managed care plans to address social determinants of health (SDoH) and offer preventative upstream interventions.
Our Network in California
Our California network spans the entire Golden State and Californians, community-based organizations (CBOs), and more than 71 customers across the state are already using our platform to find and connect to needed services and support.
- 3,005,249 users statewide
- 9,498,815 searches statewide
- 26,378 listed programs serving California
- 4,937 claimed programs serving California

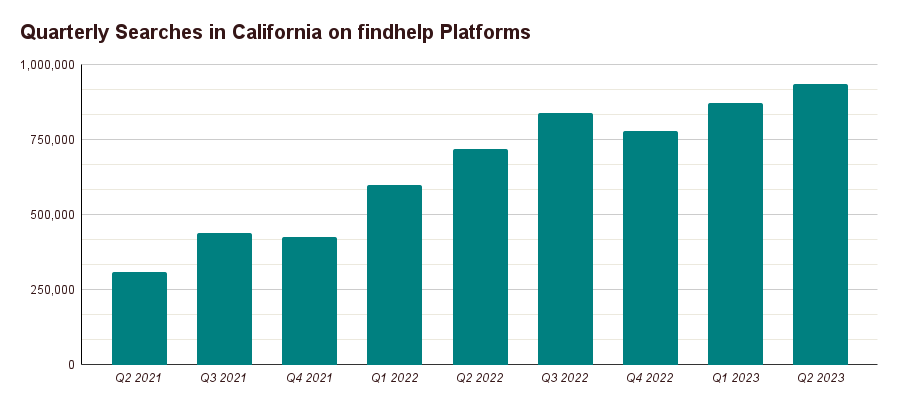
Over the past two years, monthly users and searches on Findhelp’s network in California jumped 453% and 204% respectively, reflecting our important (and growing) role in connecting Golden Staters to local social assistance.
Collaborating to Support CalAIM
We partner with managed care plans throughout the state to support the CalAIM initiatives. Our technology provides both the platform to connect with contracted partners and support for billing, invoicing, and reporting. Throughout the CalAIM process, our Customer Success team works with the managed care plan staff to onboard them to the Findhelp CalAIM platforms, including detailed training sessions, office hours, in-person support, and more.
At the same time, our Community Engagement team works with the contracted service providers to onboard them to the platform. This includes in-person and virtual support to claim their programs, turn on referrals, set up screeners, and submit data for billing purposes.
Typical CalAIM Workflow
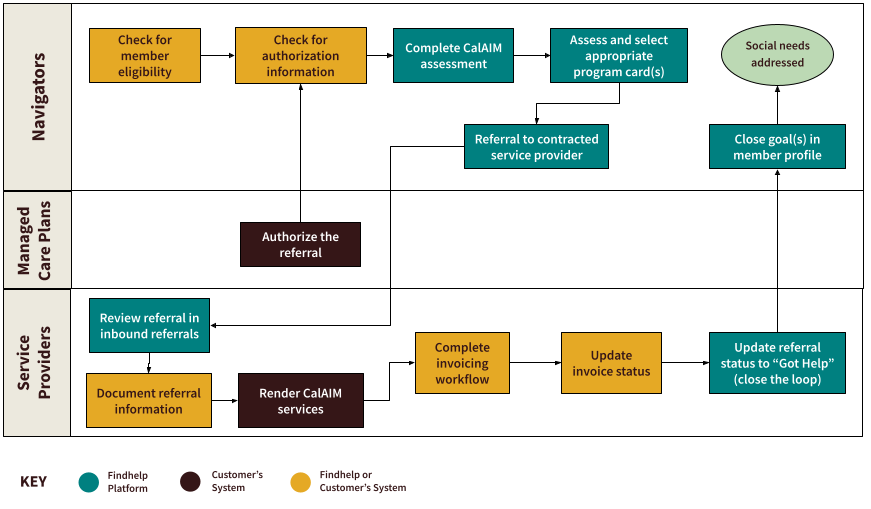
- Managed care plan navigators complete a required eligibility check to confirm the person being helped is qualified for CalAIM; this can occur in either Findhelp or the managed care plan’s provider portal or care management system.
- A navigator completes the CalAIM Assessment in Findhelp to collect member information and indicate the member’s needs across the 14 service categories.
- Available services are displayed in Findhelp based on the member’s assessment responses. The navigator then chooses the appropriate program and makes a referral to the service provider.
- The managed care plan will authorize the service; the authorization can be accessed either in Findhelp or the plan’s provider portal.
- After completion of the eligibility check and authorization for services, the referral is updated via the Findhelp platform to the service provider, indicating the member can now receive services.
- After addressing the member’s need, the service provider closes the loop on the referral, then fills out the data form in Findhelp to facilitate simple billing.
- Findhelp creates and sends an invoice to the managed care plan on behalf of the service provider.
Supporting California Customers & Seekers
Findhelp collaborates with managed care plans across the state to connect Californians to resources via CalAIM. We enable their staff to order more than 445 different social services from community partners. Through the Findhelp platform, navigators can assess members and order services based on state-mandated eligibility criteria, and service providers can bill for and receive payments. Furthermore, Findhelp’s data and analytic tools can be used by our customers and partners to identify gaps in services and provide actionable insights to inform public policy and prioritize initiatives.
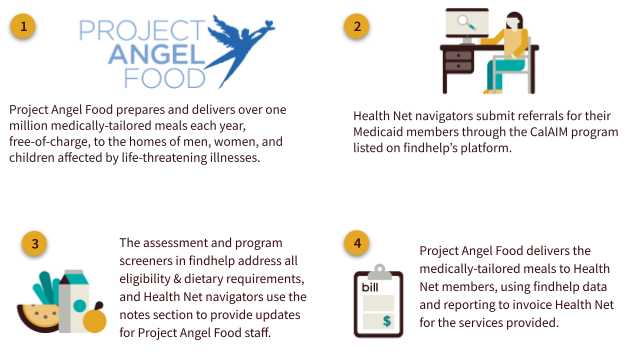
Here are just a few examples of how we’re partnering with California organizations to support their CalAIM programs.
Founded in California more than 40 years ago, Health Net believes every person deserves a safety net for their health regardless of age, income, employment status, or current state of health. Health Net provides quality affordable health plans for individuals, families, Medi-Cal members, Medicare and businesses. Health Net launched their CalAIM platform Community Supports (powered by Findhelp) in 2021.
- Health Net works with Findhelp to manage their CalAIM-related referrals and workflows. Our platform allows for end-to-end referrals in tandem with existing workflows in Health Net’s internal care management system and provider portal. Health Net has a mixed workflow: navigators check the provider portal for eligibility and service providers use the Findhelp platform.
- We partner with Health Net to onboard service providers to Findhelp’s invoicing process. Our Community Engagement team has worked extensively with more than 100 of Health Net’s contracted community providers to onboard them to the platform and ensure they claim and accept referrals. Our Customer Success team works ongoing with Health Net’s staff to provide training, office hours, and general support of the platform.
As a local, public, not-for-profit managed care health plan, Alameda Alliance for Health is committed to making high-quality health care services accessible and affordable to Alameda County residents. The Alliance staff and provider network reflect the county’s cultural and linguistic diversity; they launched their Findhelp platform in 2023 to provide social care support for county residents.
- The Alliance works with us to manage their CalAIM referrals and internal staff workflows. Similar to Health Net, the Alliance has a mixed workflow, with staff checking internal Alliance systems for eligibility and authorization and navigating for services via the Findhelp platform.
- After authorization of the service occurs through internal systems, Alliance staff use the Findhelp platform to send referrals to service providers via our marketplace functionality. Service providers also identify eligible members and make referrals to Alliance’s internal Community Supports and Case Management teams, via Findhelp program listings.
Supporting communities for over 30 years, Aetna Better Health of California brings national experience to the local level, ensuring members have the resources and tools to stay well; they launched their CalAIM platform (powered by Findhelp) in 2021 to connect members to community resources.
- Aetna has collaborated with Findhelp to build automation into their end-to-end referrals workflow. Their staff navigators can identify at the start if a person is eligible for services, and shared demographic data helps to avoid double-documentation.
- Additionally, we created data collection forms for each service provider to add information from a pre-made list, such as Healthcare Common Procedure Coding System (HCPCS) codes, modifiers, and more. This allows service providers to generate and send invoices to Health Net, via the Findhelp platform.
The Future of the Findhelp’s Support for CalAIM
We continue to expand and adapt our CalAIM support in partnership with our customers, to reflect ongoing changes in the state policy landscape. Recent updates and improvements include:
- Outcome Tracking Improvements
- Service providers can document services rendered on multiple outcome tracking forms to allow for a more frequent billing cadence or separation of data collected for different uses.
- Users can save outcome tracking forms as a draft without having to enter required fields.
- Integrations & APIs
- We’re implementing additional integrations with nonprofit care management systems.
- We completed integrations with HarmonyHealth, a company that provides text messages for seeker outreach, to directly engage with those who need additional help and to support the closure of more referral loops.
- We’re making ongoing improvements to eligibility file ingestion with the capability to support member eligibility APIs.
- Authorization Workflows
- Findhelp is working with managed care plans to support their authorization workflows in deeper ways, ensuring ease of use for contracted providers and staff.
CalAIM Success Story
Want to Learn More?
Schedule a demo with us to see how we can partner with your organization to support your members via CalAIM (or other Medicaid 1115 waiver programs).