NY 1115 Waiver Program: Meeting the Needs of New Yorkers
More than 30 healthcare, health plan, nonprofit, and other organizations across New York have already implemented social care coordination platforms with Findhelp and are ready to hit the ground running when the NY 1115 waiver program is approved later this year. Read on to learn about proven strategies from some of our current New York customers and successful 1115 waiver programs across the country.
Innovating Medicaid Delivery to Address Social Needs
Why are folks talking about 1115 waivers, and what are they? Section 1115 of the Social Security Act gives states flexibility to design and improve their Medicaid programs by providing waivers authorizing experimental, pilot, or demonstration projects.

1115 waivers are initially approved for five years and can be extended for three to five more years. Many states focus their projects on addressing Medicaid enrollees’ unmet health related social needs and the downstream health impacts.
At Findhelp, we have both a history of successful Medicaid 1115 waiver support and deep relationships across the state of New York and beyond. Our technology supports:
- Capturing eligibility and authorization needs
- Reporting on services rendered, codes, and data needed for invoicing and claims
- Facilitating invoices and payment to community organizations and vendors
Our Network in New York
One of the reasons our customers across industries choose Findhelp is because we have an engaged network that’s already in place. Our network spans the entire Empire State and New Yorkers are already using our platform to find and connect to needed services and support.
- 1,530,721 users statewide
- 4,905,024 searches statewide
- 13,710 listed programs serving New York
- 2,034 claimed programs serving New York
Findhelp’s data and analytic tools can identify gaps in services and provide actionable insights to inform public policy. For example, over the past two years, monthly users and searches on Findhelp’s network in New York jumped 452% and 153% respectively, reflecting our important (and growing) role in connecting Empire Staters to local social assistance.
Partnering to Help New Yorkers
As of September 2023 we partner with more than 30 customers throughout the state to connect their patients, members, students, constituents, and clients to local resources. Our customers know that they can trust us to help them connect their most vulnerable populations to resources and services that can help them, as shown by our Best in KLAS rating for 2023.

A few of the organizations we partner with in New York.
These highlights show how some of our customers successfully partner and innovate with us to lift up their communities.
New York City’s Institute for Family Health (IFH) is a federally qualified health center (FQHC) that launched their IFH Findhelp platform in August 2019 to foster meaningful connections between their patients and CBOs like A-Med Supplies, God’s Love We Deliver, Preferred Home Care, and many more. By partnering with Findhelp to build this trusted network of community partners, 94% of IFH referrals receive a response from the referred-to CBO.
In 2021, IFH deepened our partnership by leading an innovative collaboration between Findhelp and UberHealth to provide 2,396 free rides for patients to and from vaccination centers during the COVID-19 pandemic. IFH continues to explore additional innovative approaches to proactive social care and plans to launch additional Findhelp-UberHealth transportation assistance programs in 2024 to ensure patients can attend routine medical care appointments.

Value Network LLC, IPA is a behavioral health care collaborative in Western New York that advances healthy equity, innovation, and transformational strategies. They launched the Value Network Community Connector platform (powered by Findhelp) in December 2021 to facilitate stronger coordination between helping professionals, patients, and the greater Western NY community.
Value Network has used their vast network of providers to strengthen the safety net to address member’s social needs and has led the way with innovative work to create efficiencies in provider workflows by integrating multiple electronic health record (EHR) systems with Findhelp.

Mount Sinai Health System uses their Community Resources Guide (powered by Findhelp) to support all their patients in need and connect them to free or reduced-cost social services with dignity and ease.
Since launching the platform in December 2019, more than 85,000 patients and staff have visited the platform to search the 13,000+ programs available in Findhelp’s New York network. Mount Sinai continues to build robust community relationships and generate social care referrals with an array of partners to holistically support the social needs of their patients.

A Legacy of Support for Medicaid 1115 Waivers
We’ve been partnering with our customers and trusted community partners to support Medicaid 1115 waiver programs since 2019 in Massachusetts and California, and are uniquely positioned and ready to support New York’s Medicaid 1115 waiver. We collaborate with health plans, managed care organizations, accountable care organizations, and community-based organizations to configure workflows and payment processes to fit the requirements of each state’s program.
Massachusetts: Flexible Services

In response to increasing needs surrounding food, housing, and behavioral health, Massachusetts’ department of health, MassHealth, launched their 1115 demonstration waiver program, Flexible Services, in 2019.
Under Flexible Services, MassHealth pays for health-related nutrition and housing supports for certain members enrolled in an Accountable Care Organization (ACO). These ACOs pilot evidence-based approaches that address a member’s health-related social needs with the goal of improving health outcomes and reducing the total cost of health care for the member.
- Starting in 2020, Findhelp partnered with Mass General and Brigham and Women’s Health to launch Flexible Services pilots with 10 community-based organizations.
- Midway through 2020 we expanded our partnerships to include Boston Medical Center and SouthCoast Health and trained 7 additional community organizations to improve food and housing outcomes across the state.
- Today, we are partnering with several Flexible Service ACOs to support navigation assistance for areas with higher volumes of eligible patients. In the first year of Flexible Services, 99% of patients reported that their participation improved their overall health.
California: CalAIM

On January 1, 2022, the California Department of Health Care Services launched the California Advancing and Innovating Medi-Cal (CalAIM) program, an 1115 waiver program to make Medi-Cal more equitable, coordinated, and person-centered. The program covers one-third of Californians and perinatal care for half of annual births and will impact the lives of over 14 million Californians.
CalAIM expands community-based approaches to addressing complex care for high-needs populations, such as individuals experiencing homelessness, serious mental illness, or substance use disorders, or children involved in the child welfare system. Designated navigators coordinate members’ physical and behavioral care, as well as access to critical social services.
- Through 14 services such as Asthma Remediation and Housing Navigation Support, CalAIM encourages Medi-Cal managed care plans to address social determinants of health (SDoH) and offer preventative upstream interventions.
- Findhelp partners with managed care plans across the state like Aetna Better Health, Health Net (Centene), and Alameda Alliance for Health to support CalAIM. We enable their staff to order more than 445 different social services from community partners.
- As we continue to onboard new community organizations and train managed care plan staff on use of the platform, we’ve seen a 40% increase in the number of referrals sent on CalAIM Findhelp sites from July to August 2023.
Looking Ahead to 2024
Our robust data and analytics show what New Yorkers have searched for over the last two years, painting a picture of how needs have changed over time and what gaps currently exist in New York communities.
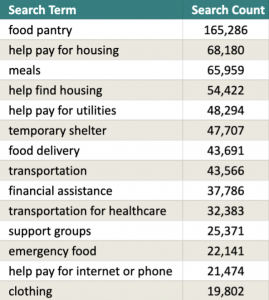
As you can see, food, housing, and transportation-related needs are among the most common for New Yorkers over the past couple of years. Findhelp has experience partnering with customers across the country to address needs like these, whether it’s via our fulfillment program, Marketplace, by establishing trusted networks of community service providers, or by collaborating with organizations like Uber Health.
When the New York Medicaid 1115 waiver is approved later this year, we’re ready to partner with our existing and future New York-based customers to help them connect their patients, members, students, and clients to helpful resources.
We look forward to collaborating with our existing customers and community partners to advance the work of the New York State Department of Health to connect people in need to the programs and services that can help them; we’re ready to support New York’s Medicaid 1115 waiver.
Partnering for Success
You don’t have to start from scratch with your pilot demonstrations; chat with one of our team members to learn how we can collaborate with your organization to successfully implement New York’s 1115 waiver program, using established best practices and our proven strategies.
- Prospective Customers: connect with our Director of Enterprise Sales, Rachel Harris ([email protected]).
- Community Organizations: reach out to our New York Community Engagement Manager, Colton Navel ([email protected]).
- Policymakers: connect with our Regional Director for Government Relations, CG Niquette ([email protected]).

