Live from New York: How SCNs Connect 1.5 Million Patients to HRSN Services
On January 1, 2025, we successfully went live with three partner Social Care Network (SCNs)—SOMOS Community Care, Forward Leading IPA, and Western New York Integrated Care Collaborative—to address the health-related social needs (HRSNs) of more than 1.5 million New York Medicaid members and pay community-based organizations (CBOs) for approved services.
Findhelp’s implementation with its partner SCNs was on-time and on-budget, meeting all of the data ingestion, platform, user experience, and interoperability requirements from the State’s 200-page operations manual.
In only six months…
Cumulatively, the SCNs have:
- Completed HRSN screeners for more than 60,000 NY Medicaid members
- Assessed 6,400 individuals to determine eligibility status
- Made 17,000 referrals for patients to local social care resources
- Received 2,700 reimbursement requests from participating community organizations for delivered services
- Reimbursed contracted community-based organizations (CBOs) and others with $785,000 for provided services, including care management and Medically Tailored Meals
Findhelp has:
- Onboarded 775 organizations (both CBOs and healthcare providers) and implemented branded Findhelp platforms in partnership with the SCNs
- Added 800 new social service programs to our network
- Supported more than 2,700 new users who have searched for help on our SCN partners’ Findhelp platforms
In this post, you’ll learn how:
Findhelp technology enables waiver workflows
We support secure data sharing and interoperability pathways
Findhelp’s SCN partners & New York network are making a positive impact statewide
How Findhelp supports a complex waiver program
New York’s prescriptive Medicaid 1115 waiver workflow requires SCNs and their partners to conduct specific activities. These requirements ensure that Medicaid members receive the right services in the right place at the right time.
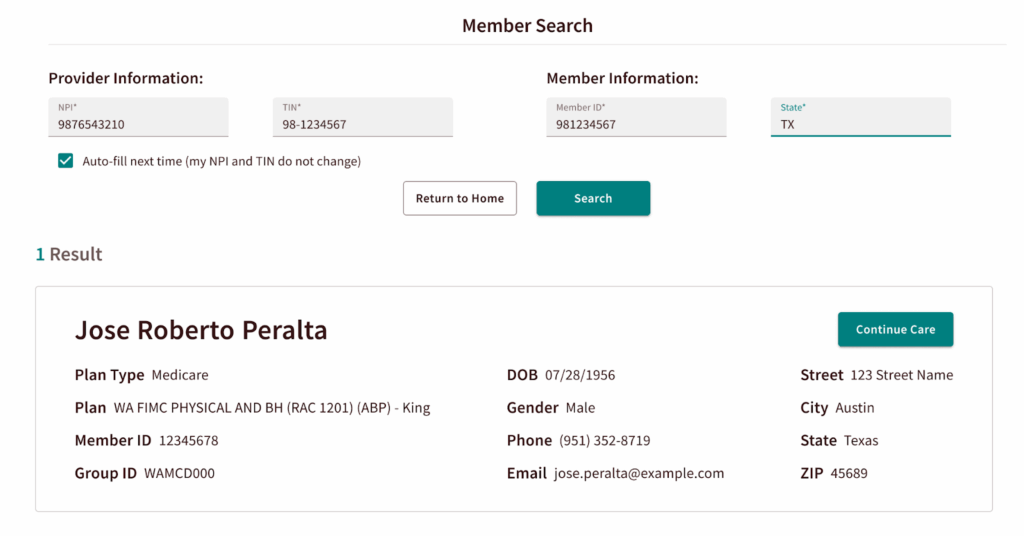
Medicaid member and eligibility lookup
To fulfill the state requirement of tying individual members to eligible services, Findhelp securely ingested the eligibility rosters of over a million New York Medicaid members served by their SCN partners. SCNs query the files to find the member. Once identified, the member’s profile immediately displays their waiver eligibility status, streamlining the first step of the workflow.
Screening and eligibility forms
Findhelp has also embedded New York’s required eligibility assessment, which determines whether members meet service eligibility criteria.
New York’s required screening tool is embedded in the Findhelp platform for SCNs and their partners to identify Medicaid members with needs at scale.Additionally, Findhelp ingests HRSN screening results from EHRs for healthcare organizations that are participating in the waiver. This enables the healthcare partners to continue their typical workflows while contributing to this important work.
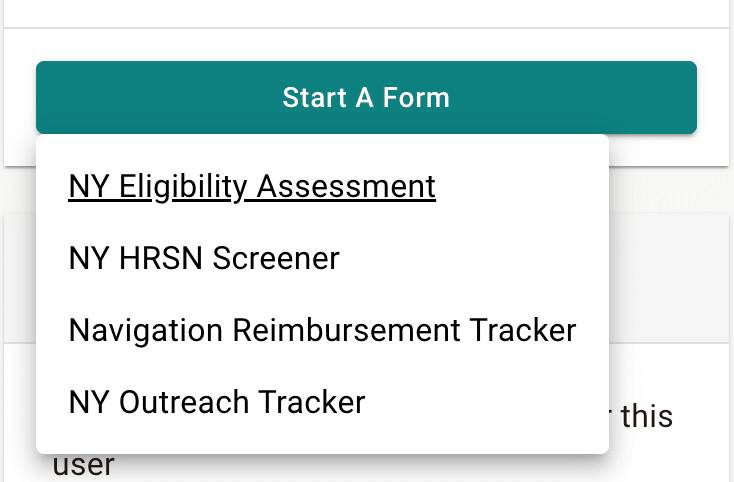
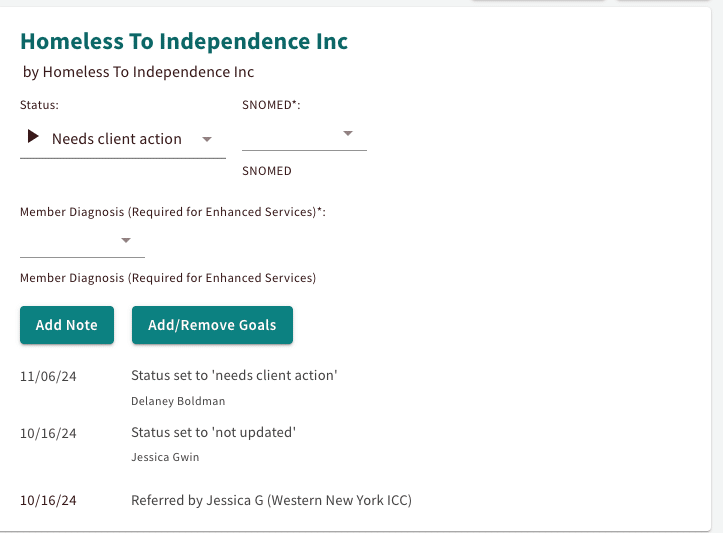
Closed-loop referral tracking
After SCNs and their partners have identified a member’s need(s), they can send closed-loop referrals to CBO partners in their contracted network. Using Findhelp’s tiered network approach, SCNs can also send referrals for services that may not be covered by the waiver, but that are still important for the member’s wellbeing.
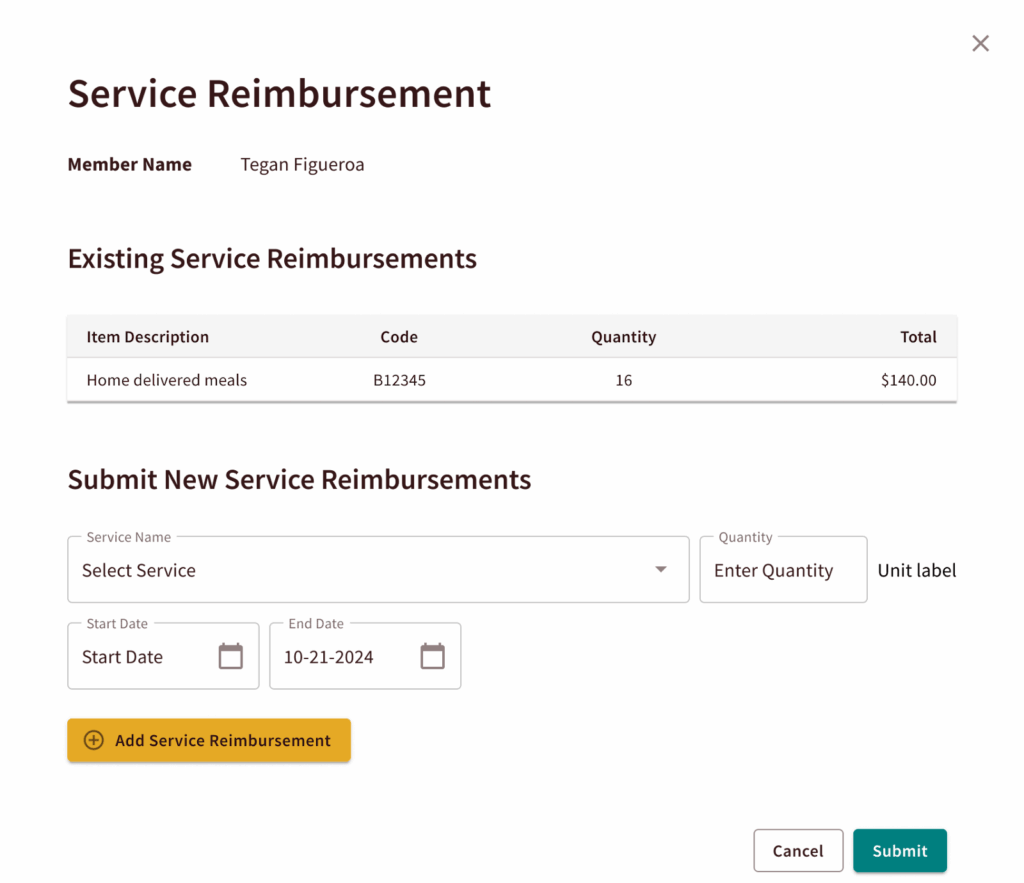
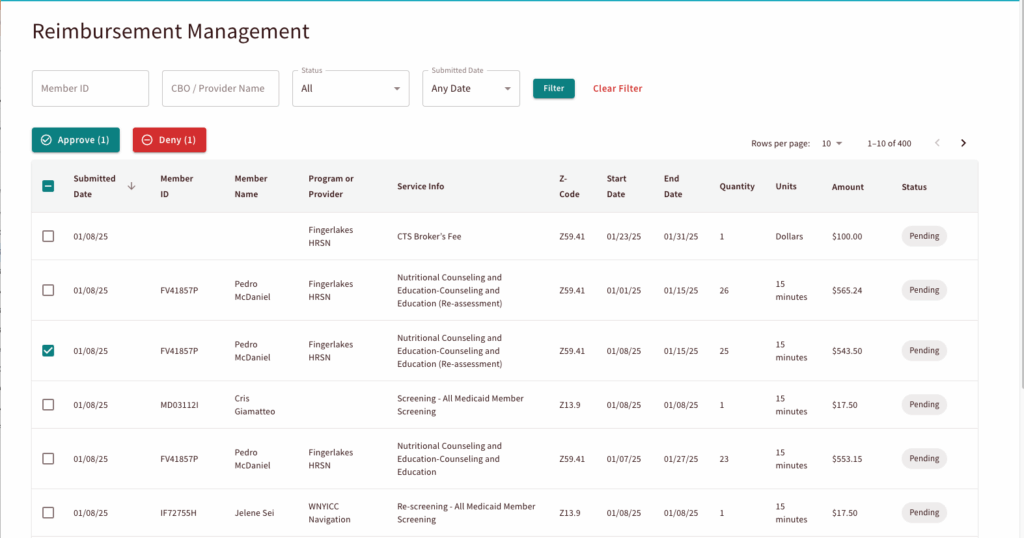
Claims submission and payment
SCN partners use Findhelp to document the waiver services they have provided. Findhelp enables social care invoice requests and claims that include standardized codes for services provided. The SCNs use Findhelp to manage payments, while CBOs can use Findhelp to track payment for the services they provided.
Reporting and analytics
Screening, referral, and services activities are mapped to standardized social care codes for consistent and accurate reporting that meets state and CMS requirements.
The power of connection & interoperability pathways
A core requirement of the waiver is seamless data sharing. To achieve this, Findhelp established a first-of-its-kind, direct connection with New York’s health information exchange (HIE) built on modern, federally-recognized data standards. Our approach moves beyond legacy methods, embracing HL7® FHIR® (Fast Healthcare Interoperability Resources) to ensure social care information flows securely and efficiently between SCNs, healthcare providers, and the State.
We use FHIR Bundles to exchange information. A FHIR Bundle acts as a standardized digital package, containing all relevant data for a specific interaction—such as a member’s screening results, subsequent referrals, & service updates—in a single transaction. This method offers significant advantages:
- Speed and efficiency: Bundling information dramatically reduces the number of connections needed to share a complete picture of a member’s journey, enabling near real-time updates for care coordinators and providers.
- Standardization: FHIR is the national standard for healthcare data exchange. By using FHIR, we ensure that data from the Findhelp platform is instantly usable and understandable by hospital electronic health records (EHRs) and other clinical systems. This aligns with the work of national efforts like the Gravity Project, which champions the use of FHIR for HRSNs.
- Enhanced coordination: For members who have consented to sharing, this robust data exchange means a provider can see HRSN screening results from our platform directly in their own system. This timely insight facilitates integrated care planning and whole-person care.
“This implementation is a true testament of our mission to connect all people and the programs that serve them, with dignity and ease. We’re excited to continue working with our Social Care Network partners to expand access to care for New York’s Medicaid members.”
Mukta Nandwani
Chief Technology Officer at Findhelp
Stronger together: Meet our partner Social Care Network (SCNs)
SCNs are new entities tasked with managing social care delivery for people with Medicaid under the state’s Section 1115 Medicaid health-related social needs (HRSN) waiver demonstration. Findhelp provides interoperable and integrated technology to three SCNs, fundamentally changing HRSN service delivery in New York.
A major part of the state’s HRSN service delivery infrastructure, these SCNs are screening for needs, navigating people to services, building CBO networks for effective service delivery, and paying contracted CBO partners for services.
SOMOS Community Care
A network of over 2,600 culturally competent healthcare professionals, SOMOS Community Care provides care to over 1 million patients, and their mission is to expand equity in healthcare for the most underserved communities in New York. SOMOS’ SCN serves the Bronx in New York City.

“After many months of accelerated implementation, SOMOS is excited that the program is live. Our network of CBOs, primary care physicians and other providers have been helping patients with their social needs at various degrees for years! It’s amazing that there is finally a program that connects social care to medical care and that there’s a recognition for the need. Our partnership with Findhelp will formalize and scale this process to meet the needs of 700,000+ Medicaid members in the Bronx. Tremendous work was happening all around, but we’re grateful for the time and effort from Findhelp to make this happen timely.”
John Dionisio
Chief Information Officer at SOMOS
Forward Leading IPA (FLIPA)
FLIPA’s integrated delivery network is the first in upstate New York to unite behavioral health, social care, and primary care under one umbrella, and their mission is to strengthen healthcare through meaningful connections. Their SCN, “WeLinkCare”, serves the Finger Lakes region of upstate New York.

Western New York Integrated Care Collaborative
WNY Integrated Care Collaborative partners with healthcare plans and providers to improve patients’ health in Western New York. Through their regional service-provider network of community-based organizations, they provide comprehensive, cost-effective, community-based integrated care. Their SCN, “The Integrated Care Network”, serves Cattaraugus, Chautauqua, Erie, and Niagara Counties in western New York.

Our statewide New York network
One of the reasons our SCN partners chose Findhelp is because we have an engaged network that’s already in place. Our network spans the entire Empire State and millions of New Yorkers are using our platform to find and connect to needed services and support.

In total, more than 12,700 programs serving New York are listed on the Findhelp platform, providing important and necessary services to New Yorkers, from food support, housing assistance, and legal aid to transportation, health care, and beyond.
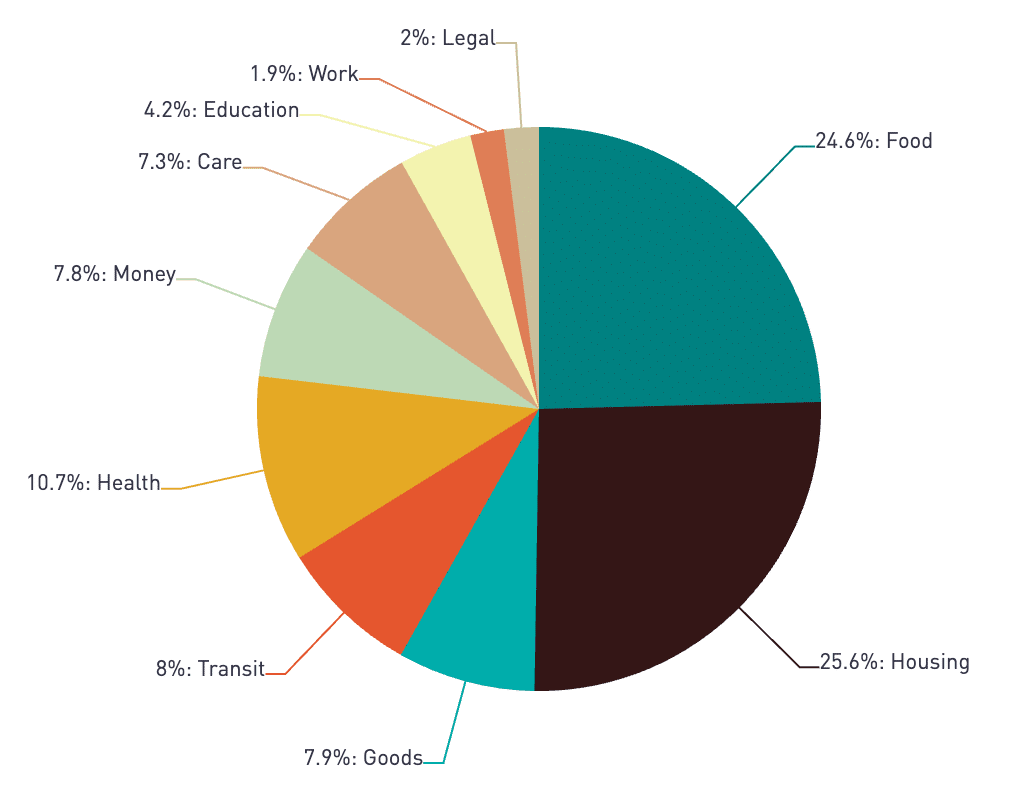
Searches made in New York ZIP codes, by category of need
In the past two years, from July 2023 to June 2025, our platform supported 1.9 million New Yorkers with:
- 5.8 million searches for resources
- 315,000 referrals to CBOs
- 677 programs newly claimed by their host organizations
Next steps for the SCNs
Over the next two years, these SCNs will access eligibility information, screen for needs, make closed-loop referrals, pay for services, and report on outcomes for all members within their regions. Findhelp will continue to provide best practices, guidance, and platform optimization to meet their needs. These deep partnerships will power a safety net for Medicaid members, in collaboration with regional healthcare providers, community-based organizations, and others.


We recently brought our partner SCNs to our headquarters in Austin, TX, to collaborate on best practices and align on a shared roadmap for the rest of the year.
Over the next year, Findhelp is committed to enhancing our support for waiver workflows:
- Integrating the Medicaid Eligibility Verification System (MEVS) for faster eligibility determinations
- Optimizing reimbursement workflows to decrease administrative burden
- Fine-tuning SCN navigator workflows to increase operational efficiency
Findhelp has a history of successfully supporting Section 1115 waiver demonstrations and statewide HRSN service delivery across the country, from California to Massachusetts, Indiana, and beyond. We’re proud to partner with these SCNs to provide interoperable and integrated technology that will fundamentally change HRSN service delivery in New York.
Ready to support HRSN service delivery and reimbursement
We’re ready to help. Connect with our team to explore how Findhelp can support social care service delivery.