Redetermination and Community Engagement Requirements from Beginning to End
Our platform takes the complexity out of redetermination by connecting states, beneficiaries, and MCOs with our nationwide network for a single, end-to-end solution.
A fragmented process costs time, money, and members
Managing redeterminations and new community engagement mandates is disconnected. This fragmented system leads to low completion rates (as low as 40%), high administrative costs, and members losing coverage—even when they are still eligible.
1
State administrative burden
States face soaring administrative costs from increased manual verifications, call center surges, and new IT system demands.
2
Navigator disconnect
Navigators lack the real-time visibility and unified data needed to verify services and hours, leading to fragmented communication and support.
3
Beneficiary confusion
Beneficiaries are confused by complex policies, waiver and exemption management, and the need to navigate multiple disconnected systems.
Activate, don’t build: A single, integrated platform
Our platform connects a smart eligibility-check with our nationwide network of community partners, allowing states to keep members covered and promote economic mobility in one unified solution.
From Policy to Practice
Intelligent Segmentation
Avoid the cost of repeat messaging and focus resources only on members who require action.
Eligibility
Check
Initiate proactive outreach and securely collect member data to personalize their
redetermination path.
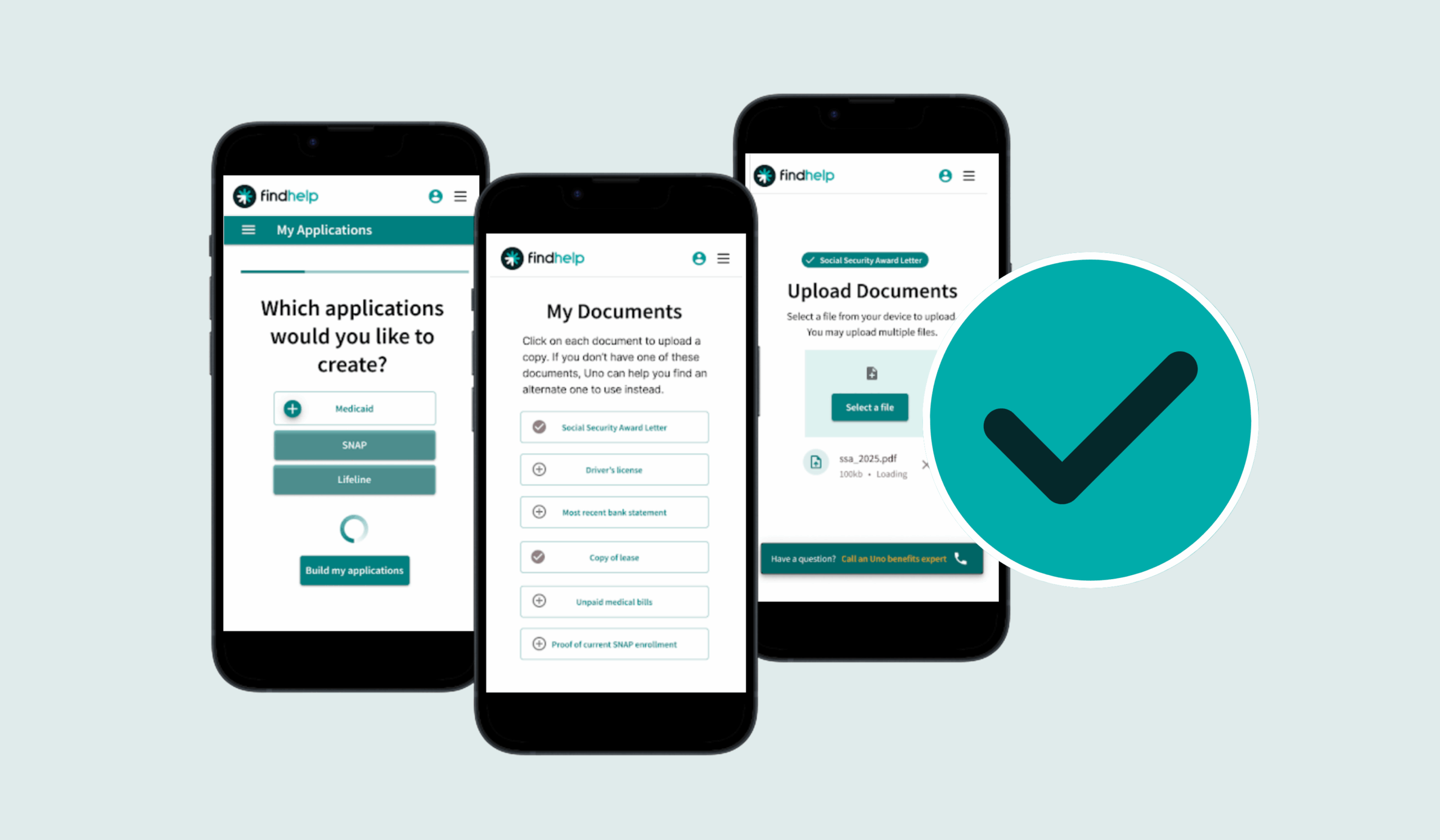
Redetermination Support
Provide a unified portal for members, navigators, and MCOs to manage the renewal process and track progress.

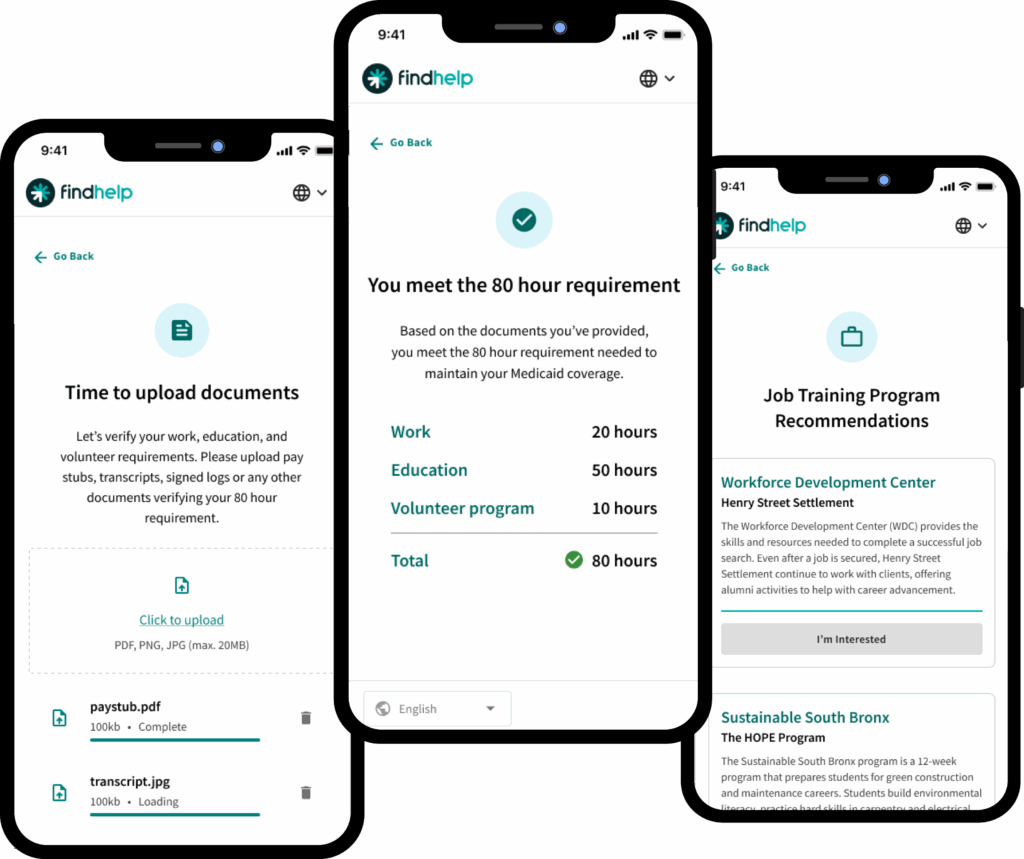
Navigation & Connection
Leverage auditable, closed-loop referrals to job training, volunteer opportunities, and educational programs.
Reporting & Verification
Provide trusted third-party verification and outcomes tracking to support compliance and reporting.
What makes us different? Our integrations.
We leverage data and integrations to drive ex parte verification and reduce burden on states, MCOs, and beneficiaries.
A Cost Effective, Proven Partnership
Leverage the platform with the biggest reach and biggest impact that is already built, paid for, and delivering proven results.
85% Completion Rate
Achieve an 85% completion rate (up from 40-50%) and see a 10% increase in member retention.
Member Reach
Leverage the only platform that works with 70% of the nation’s MCOs, reaching more than 90% of Medicaid members.
190 MCO Partners
Our existing partnerships with 190 MCOs (out of 282) drastically reduce implementation timelines and build costs.
Safe and Secure
Ensure total data integrity and security on a platform that is fully HITRUST-certified and HIPAA-compliant.
See the platform in action
See how the Findhelp platform unifies states, MCOs, and navigators to ensure compliance, control costs, and create real pathways to self-sufficiency.