Findhelp Acquires Uno Health and Is the First Social Care Platform with Benefit Enrollment
Big news: We’re thrilled to announce that Findhelp has acquired Uno Health, a top-tier digital platform for government benefit enrollment. The goal: make it dramatically easier for people to get the benefits they deserve and help our partners—states, payers, and providers—manage the process more efficiently.
Learn how:
This move creates the first-ever full-stack social care platform.
Findhelp will now provide end-to-end enrollment and redetermination for programs like Medicaid and SNAP.
We’re closing the gap between finding help and getting help, making it easier for people to enroll and stay enrolled.
Benefit eligibility, enrollment, & redetermination made easy
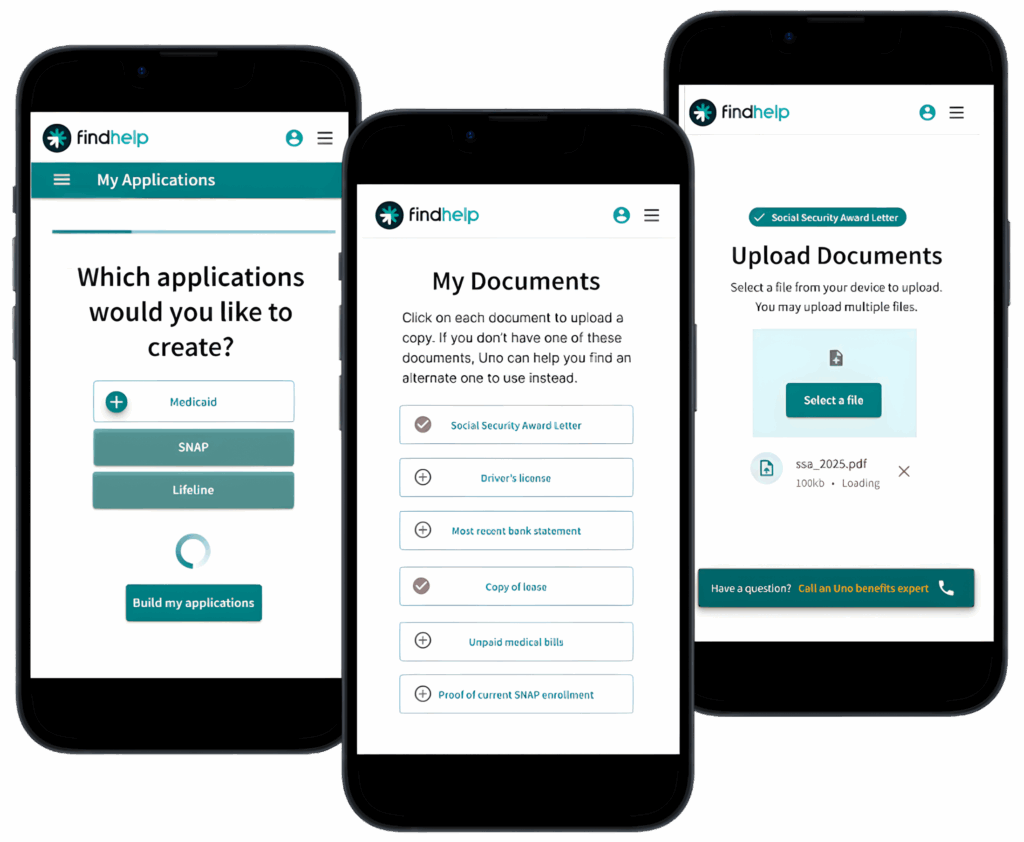
As a digital enrollment platform for government benefits, Uno Health simplifies the end-to-end eligibility, enrollment, and redetermination process for programs like Medicaid, SNAP, TANF, and other key income and employment-based benefits.
With this acquisition, Findhelp is the first social care platform to enable rules-based eligibility assessments, closed-loop referral capabilities, application creation, enrollment submission, and recertification—all in one comprehensive longitudinal record.
- All-in-one support: One simple digital process for checking eligibility, applying, and handling renewals for all major income-based programs.
- Flexible help: Pick the support level you need, from free, do-it-yourself screeners to a “we’ll handle it” fully-managed service.
- Real savings, less hassle: Our digital-first approach slashes administrative costs by up to 75% and boosts document return rates by 3x.
- More people get help: Organizations using our tools see 85% or higher approval and renewal rates—nearly double the national average.

“Uno built an incredible technology to simplify this process, including: easy eligibility screenings, an intuitive document upload process, and the ability to seamlessly submit an application. Together, we’re modernizing enrollment and creating a more efficient application process for these benefits.”
Erine Gray
Founder & CEO, Findhelp
Why this, why now?
Enrolling in benefits is difficult. Every year, billions of available dollars go unused because the system is too complex, fragmented, and intimidating. On average, 30% of Americans who are eligible for these programs don’t get enrolled, leaving a staggering $80B on the table annually. People simply get lost in the paperwork.
Add to that new Medicaid community engagement requirements and redetermination policies, which are challenging states, payers, and providers to innovate. To manage these changes, stakeholders need modern solutions that are sustainable and transparent.
We’re directly addressing this national challenge by offering an integrated digital solution to help people check eligibility, apply for benefits, submit documents, and stay enrolled in critical programs. When folks can access the support they qualify for, their health outcomes and economic stability improve.
A “full-stack” solution: What’s included?
Adding these new capabilities to Findhelp’s technology creates the first true full-stack social care platform. It streamlines every step of the journey: eligibility checks, document collection, application submission, and redetermination across 10 core income-based programs.
Here’s a look at what makes our platform so different:
- End-to-End Enrollment: Our comprehensive solution manages everything from eligibility checks to application submission and tracking, keeping people informed along the way.
- Fast, Digital Experience: The eligibility check takes only 60-90 seconds and provides a clear benefits guide for people to navigate their options.
- Intelligent Document Collection: The rules engine knows exactly which documents are required for each application, making it easy for people to submit and attach the necessary info the first time.
- Flexible Integrations & Support: The platform works within existing Findhelp workflows, can be used independently, or connected to State Constituent Portals and Eligibility Systems. We offer everything from free self-service screeners to fully outsourced enrollment management.
- Better Outcomes: Organizations can achieve 85% or higher approval and redetermination rates and 85-90% enrollment success rates. This is a huge leap from the industry average of 40-50%.
- Data-Driven & Compliant: The platform is HITRUST-certified and HIPAA-compliant. It can ingest claims, exemption, and hardship data to streamline applications and reduce administrative burden.
How this helps everyone
Our solution is designed to solve real problems for our partners and customers:
Hospitals & Health Systems
Streamlined enrollment means less uncompensated care, more efficient case management, and greater coverage continuity.
Payers
Improve revenue optimization and risk capture, reduce member churn, and help boost HEDIS and STAR ratings.
Government
Simplify complex eligibility processes, cuts down on incomplete applications, and helps states meet new policy mandates while saving costs.
Connecting the dots: From a referral to real stability
Every day, millions of people use Findhelp to search for support with food, housing, and utilities. A large percentage of those daily referrals are for income-based programs like Medicaid and SNAP. But too often, that’s where the journey gets stuck—a person gets a referral but gets lost in the complex enrollment paperwork.
By embedding benefit enrollment and redetermination workflows directly into the Findhelp ecosystem, we can finally close that gap. The result is a single, unified experience that helps people not only find help but stay connected to it with dignity and ease.

“By joining Findhelp, we’re creating something truly unique… Together, we can tackle the root causes of under-enrollment at a national scale and finally modernize how benefits are accessed and managed.”
Anna de Paula Hanika
Co-Founder, Uno Health
See our benefits enrollment options in action
With a proven platform, thriving network, and tailored solutions, Findhelp is powering the foundation for a better social safety net—schedule your demo today and see for yourself.