Part 1: A Blog Series on the Highly Anticipated CHRONIC Care Act
How Non-Medical Benefits Will Become Free
by Bella Kirchner, Special Projects Manager
Healthcare costs in the United States are the highest in the world and are continuing to rise. On average, the US spends $10,000+ per person on healthcare, 31% higher than the next highest-paying country1. Because of this crisis, insurance companies, as well as Medicare and Medicaid Programs, are moving away from the traditional reimbursement model that pays for volume of services towards one that focuses on value — improving a patient’s health while reducing the cost of care and increasing satisfaction for all participants. The long-standing volume model pays based on number and type of services provided, regardless of patients’ health outcomes, quality of care, or cost to the system. With the new value model, doctors and healthcare organizations have financial incentives to keep patients healthier and control costs, which can be done by providing high-quality care and coordinating better social care. To boil it all down — keep patients healthier and you get paid more.
How Do You Keep Patients Healthier?
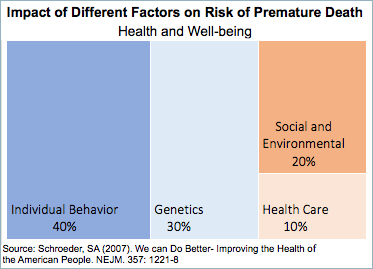
For many decades, the healthcare industry has focused on using clinical medical care (e.g., office visits, medications, hospitalizations) to improve the health of their patients. However, research shows that much of a person’s health is actually not determined by clinical healthcare, but by a person’s individual behaviors and social & environmental factors, often referred to as social determinants of health2.
Ignoring and underinvesting in these factors explains to some degree why health indicators in the US lag behind so many other countries3. When you don’t take care of a patient’s basic needs, their overall health suffers. The realization that addressing these factors has major impacts on both health outcomes and the cost of care has led to changes in both care and reimbursement models.
Can Legislation Help?
One of the most significant moves towards changing these reimbursement models was the passage of an act that affects Medicare Advantage plans. These plans are offered by private insurance companies to Medicare-eligible individuals and offer additional benefits beyond traditional Medicare, such as dental, vision, and hearing coverage. The CHRONIC (Creating High-quality Results and Outcomes Necessary to Improve Chronic) Care Act, passed by Congress on February 9, 2018, changes the way these supplemental benefits provided through Medicare Advantage plans are defined4. Previously, supplemental benefits reimbursed by CMS (The Centers for Medicaid & Medicare Services) for chronically ill beneficiaries had to be health-related services used to “prevent, cure or diminish an illness or injury.” The CHRONIC Care Act changes that definition to cover services that provide “a reasonable expectation of improving or maintaining the health or overall function of the chronically ill enrollee and may not be limited to being primarily health related benefits.” 5 This is a significant move in the industry — reimbursement for non-health services.
What Might “Non-Medical” Services Include?
Looking back at the wording, there is a lot of room for interpretation. The act simply states that the service either maintains or improves a patient’s health and does not need to be completely health related. Some examples of these services are:
- Home modifications, such as ramps, grab bars, and support stalls;
- Air conditioners for asthmatic patients;
- Mold removal for emphysema patients;
- Pest control for homebound patients;
- Food delivery for recently discharged or homebound patients; and
- Transportation to medical and social services appointments.
All of these services aim to address the social, environmental, and/or behavioral factors that impact a patient’s health outcomes.
How Can Patients’ Needs be Managed?
As the industry moves towards value (lower costs & better care), health insurance plans and healthcare organizations have realized there is a need for more intensive follow-up, coordination, and care management after the patient leaves the doctor’s office.6 Health plans and providers are hiring nurses and case managers to help coordinate the various elements that are involved in a patient’s care, while keeping an eye on managing costs, in order to lead to better outcomes.7, 8
According to the Bureau of Labor statistics, the number of care managers is expected to increase by 20 percent between 2016 and 2026.9 Currently care managers focus mostly on medical care and services, but as reimbursement models change, these are the workers who will help bridge the gap between medical and non-medical care. In addition to coordinating medical care, they’ll start working with non-profit social service providers, government agencies, and even private vendors that provide services that can be purchased on a members’ behalf. There are going to be challenges in this effort to connect patients to these services and vendors, such as:
- How does the healthcare provider (be it nurse, physician, care manager, social worker) know what services are covered?
- How do they know what resources are available and how do they vet those resources to ensure they are getting good value (reasonable cost and high quality)?
- How do they know the patient has received the service?
- How do they bill the insurance company for the service since the service has been provided outside of their care?
The Changing Landscape and the Role of Health Insurance Plans
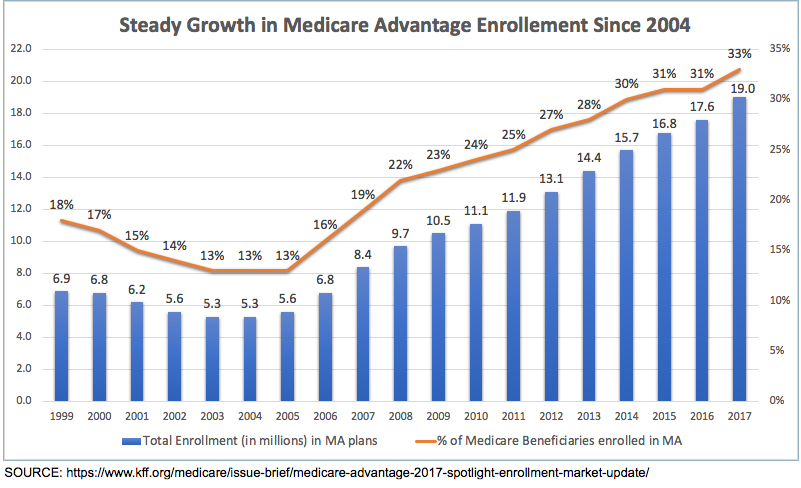
The CHRONIC Care Act only impacts reimbursement for non-medical services provided by Medicare Advantage plans, but what about the rest of the health insurance industry? Will this trend spill over to private plans? We can see that there is growing interest both from patients and payers in these new types of plans, as evidenced by the rapid growth in Medicare Advantage enrollment, which has continued to increase over the last decade (see chart).10
Why does this uptick in enrollment in Medicare Advantage plans matter in the larger scheme of the health insurance industry and value-based reimbursement? When CMS rolls out new initiatives, the private insurance industry tends to follow. This can be seen in the recent years with the overall adoption of value-based programs by private plans, following CMS’s lead.11 As CMS makes policy changes that allow for reimbursement of non-medical services, private plans are likely to start making similar changes.
When this shift happens, this means that health plans will be at the core of fulfilling non-medical needs to patients, by either acting as the facilitator between patient and service vendor or by reimbursing healthcare organizations to do the same.
Conclusion
The healthcare reimbursement landscape is changing with the realization that addressing social, environmental, and behavioral needs are key to improving health outcomes and lowering healthcare costs. Insurance companies, starting with Medicare Advantage plans, will soon be financially incented to either 1) coordinate the connection between patients and these services directly or 2) reimburse those healthcare organizations that are spending more time with patients to help them get their basic needs met.
This is all based on a bet. The bet is that if people’s basic needs are met, they’ll be healthier. If people are healthier, healthcare providers will make more money because health plans are incentivizing them to go the extra mile. If people are healthier, they’re less likely to strain resources or end up in the hospital, racking up huge medical costs.
If healthcare organizations that are talking to these patients in person every day are going the extra mile to connect with patients on a human level, and to connect patients to social care services too, like food delivery programs, or home modifications, then those healthcare organizations should realize cost savings (or bonuses). If they do realize these savings, they’ll have more money to hire case managers and care coordinators. With more case managers and care coordinators on staff there is a double bottom line effect: they make more money by helping people live healthier lives. A win for the patient and a win for the healthcare organization.
Sound a little utopian? It probably is. But we can strive for Utopia. It’s a lovely place.
Check out part two of our blog series: Which Medicare Beneficiaries Get Non-Medical Benefits?
References
2https://www.nejm.org/doi/full/10.1056/NEJMsa073350
3Woolf, S. H., and L. Y. Aron. 2013. The US health disadvantage relative to other high-income countries: Findings from a National Research Council/Institute of Medicine report. Journal of the American Medical Association 309(8):771-772.
4https://www.thescanfoundation.org/sites/default/files/chronic_care_act_brief_030718_final.pdf
5Willink, A., & DuGoff, E. H. (2018). Integrating medical and nonmedical services – The promise and pitfalls of the CHRONIC care act. New England Journal of Medicine, 378(23), 2153-2155. DOI: 10.1056/NEJMp1803292
7https://nursejournal.org/nursing-case-management/rn-case-manager-salary-and-job-outlook/
9http://samstaff.com/growing-need-case-managers/
10https://www.kff.org/medicare/issue-brief/medicare-advantage-2017-spotlight-enrollment-market-update/