Who We Serve
-
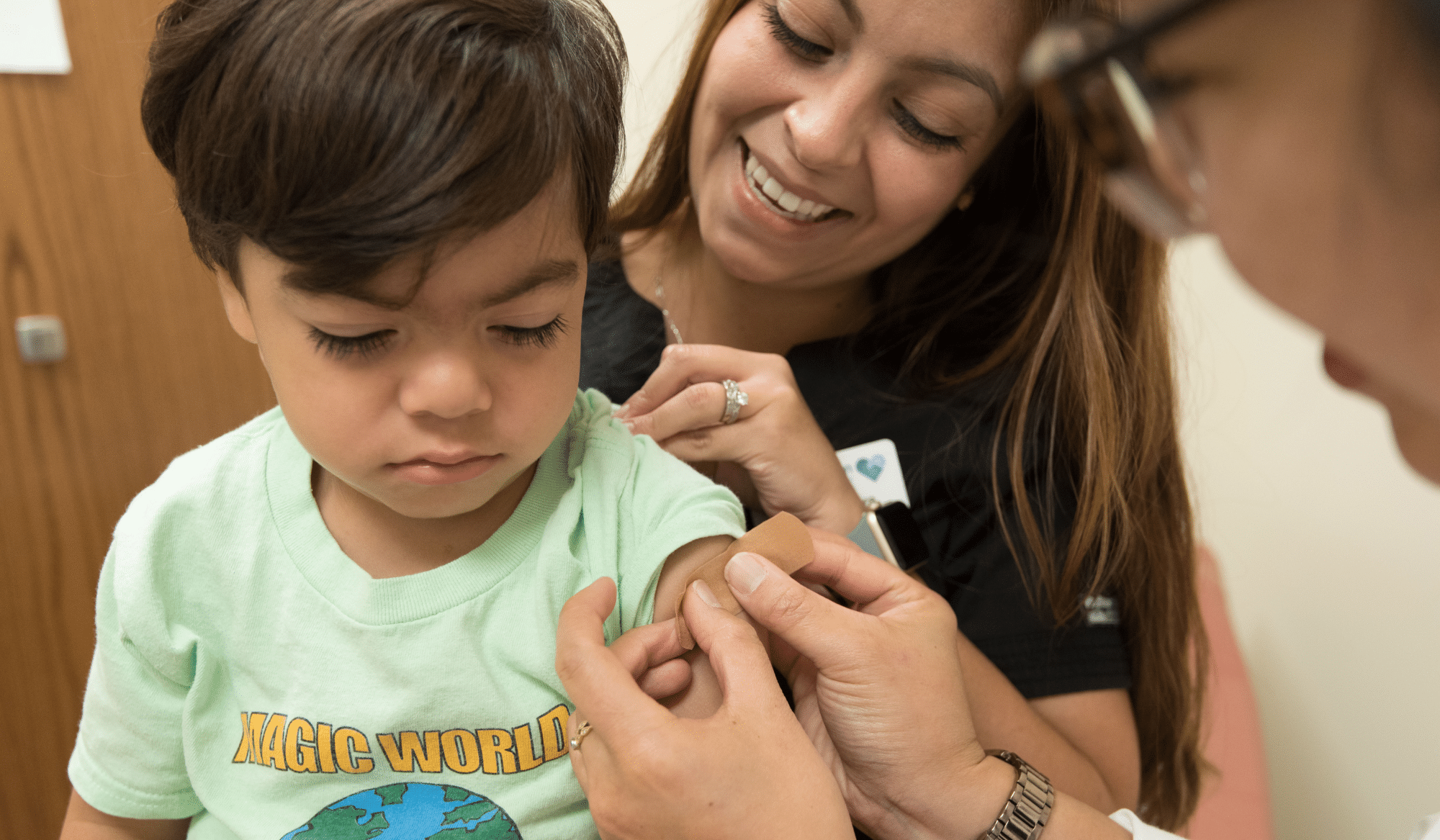
Healthcare Providers
Scale social needs screening and referrals, meet SDoH requirements, and leverage data for community strategies.
-
Governments
Improve access and track impact of government-funded programs, create targeted programs, and inform investments with data.
-
Education
Connect students and families to vital help, empower anonymous assistance, and support student success.
-
Healthcare Payers
Reduce total cost of care, boost quality scores, and gain member insights with integrated community connections.
-
United Way & 211
Enhance resource directories and easily coordinate care for more efficient call center workflows.
-
Employers
Strengthen EAPs, keep your workforce healthy, and reduce absenteeism by addressing employees’ social needs.
Become a Partner
Join the Network
Core Solutions
-
Closed-Loop Referrals
Deliver powerful programs for whole-person health.
-
Nationwide Network
Connect people to the help they need with the nation's largest social care network.
-
Reporting & Analytics
Track trends and assess your impact with robust reports and data.
-
Case Management
Manage your community program clients for free with Kiip.
Advanced Features
-
Flexible Networks
Configure your network with trusted partners and specialty networks.
-
Benefits Enrollment
Streamline benefits eligibility, enrollment, and redetermination.
-
Social Care Fulfillment
Order social goods and services for direct delivery via your Findhelp platform.
-
Integrations
Easily manage social care directly within your existing system.
Our Approach
Powered by Findhelp
-
Healthcare Providers
For providers ranging from community health centers to large, multisite systems.
-
Healthcare Payers
For all types of payers, including Medicaid, Medicare Advantage, and commercial plans.
-
State Governments
For agencies across state government, with options tailored by department and function.
-
County Governments
For counties of all sizes and budgets, from community-focused to broad regional operations.
-
K-12 School Districts
For districts of all sizes, from fewer than 5,000 to more than 45,000 students.
-
United Way & 211
For local, regional, and statewide United Way and 211 organizations.
-
For other sectors, see our general pricing.
-
For more information, talk to Sales.
Get Informed
Get Inspired
Get Involved
-
View our resource center.
-
Send us an email.
Let’s chat!
Are you looking to implement or expand your social care program? Schedule a quick call and we’ll answer all your questions!